SIDNEY – The social media phrase describing an immensely popular item or idea, “going viral,” originated from its biological counterpart, the colossal spread of something equally unpopular – viral diseases.
Social media provides one of the most expedient communication methods outside of continuous television media coverage and daily print articles.
As physical social distancing becomes the new normal in the wake of COVID-19, officials embrace social media, and social media aggregates a growing amount of data, distilling them into manageable byte-sized infographics. Social media also gives people, who may be hunkering down during this time in their homes, a chance to interact with others by sharing stories, posting content and voicing their opinions.
Potentially with this in mind, and the fact that it was pointed out that in the United States alone the term “coronavirus” surpassed 19 million Twitter mentions this month, Forbes recently published a list of the 14 most important people to follow on a national level to stay on top of COVID-19, which included Ohio’s own Tara C. Smith, professor in the College of Public Health at Kent State University. At the state level, other Ohioans also are reaching out via social media.
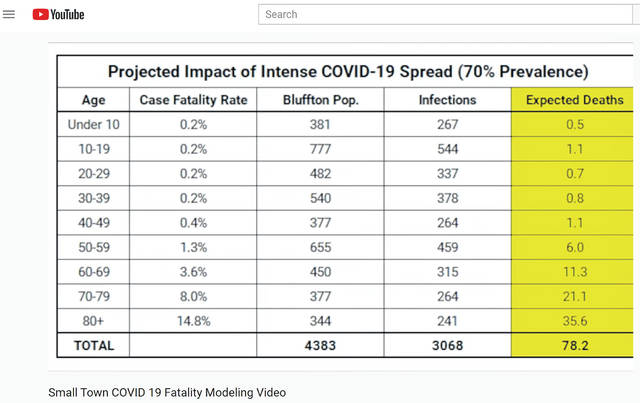
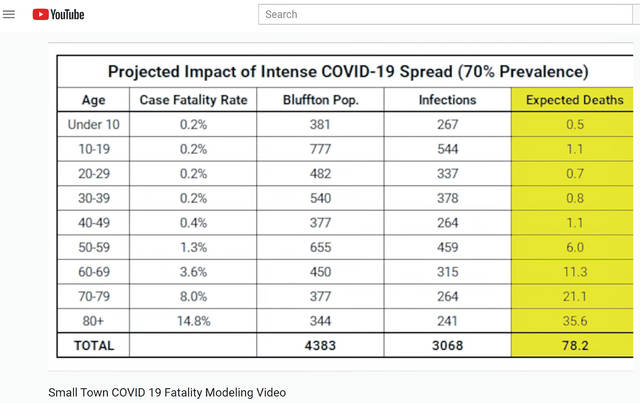
In his YouTube video, Small Town COVID-19 Fatality Modeling, Ross Kauffman, an assistant professor of public health at Ohio Northern University, extrapolated national statistics and applied them to Bluffton’s population of roughly 4,400.
In a worst-case scenario of a 70 percent infection rate, approximately 78 people in Bluffton would die, of which, three would be aged 0-49. However, starting at age 50, the number of deaths nearly doubles by decade of birth: 50-59 (six), 60-69 (11), 70-79 (21), 80-plus (36).
More than 600 people residing in Bluffton would need hospitalization, but the capacity of Bluffton Hospital, acute care facility, is a mere 25 beds.
This weekend, Ohio Gov. Mike DeWine tweeted updates from Dr. Amy Acton, director of health at the Ohio Department of Health.
“It is getting increasingly hard to give you numbers that are accurate because it is pouring in so quickly … On Saturday in Ohio there were 26 positive cases, with an age range of 31 to 86 (12 were female and 14 were male), and of these, 7 required hospitalization … as of 2 pm [Sunday] we had 36 positive cases. One of these individuals started showing symptoms in early February—so they would have been carrying it before.”
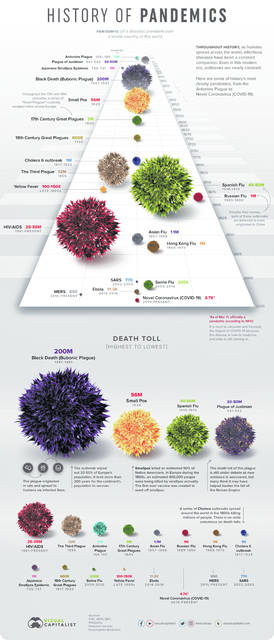
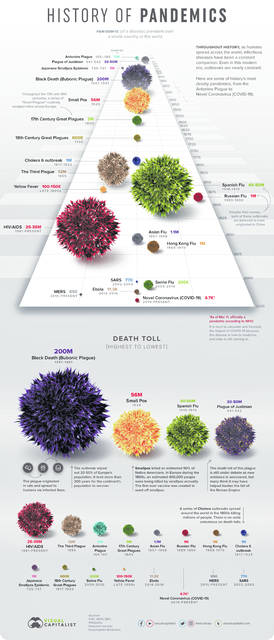
Infographics are a convenient way to encapsulate major events across large time spans to place this pandemic in its context within epidemiological history.
The largest recorded pandemic occurred in the 14th century. Known as the Black Death, or Bubonic Plague, it was caused by the bacterium Yersinia pestis that spread by flea bites. In 1928, Sir Alexander Fleming invented penicillin, a broad-spectrum antibiotic that negatively impacted the future spread of potential bacterial-borne pandemics, and it is one major reason health care professionals are actively working to prevent antibiotic resistance.
Lacking a similar broad-spectrum antiviral, pandemics in modern times mostly spread through viruses. Examples of the largest ones in the 20th century were the Spanish flu (estimated 20-50 million deaths) and HIV/AIDS (25-35 million deaths).
In the 21st century, the world experienced the much smaller swine flu (200,000 deaths). By comparison, the active novel coronavirus (COVID-19) pandemic shows fewer deaths that worldwide currently. But these numbers are growing. To figure out just how fast, epidemiologists use a statistical equation.
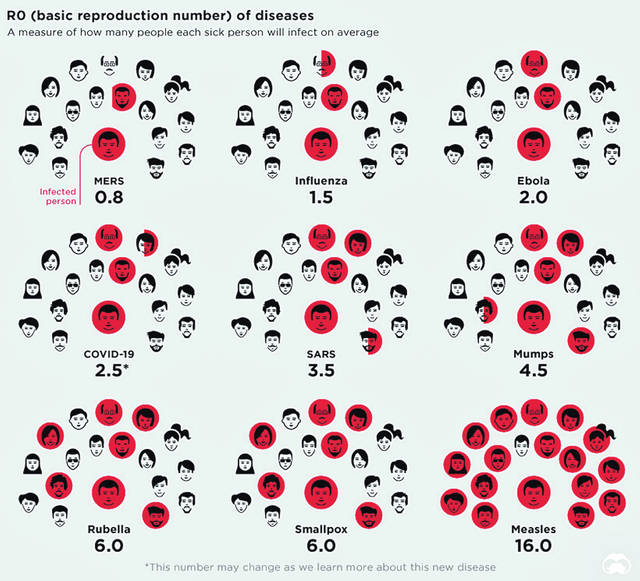
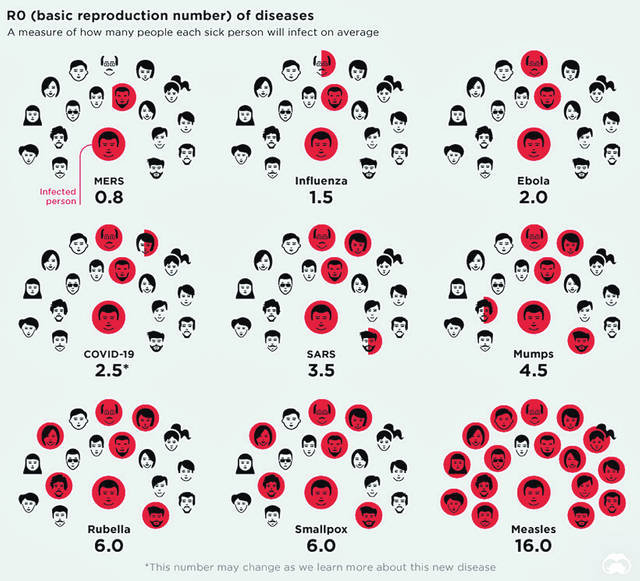
R0 (pronounced “R-naught”) is a mathematical calculation that can help predict how rapidly a disease will spread. One of the major factors is the contact rate, which is why the practice of self-isolation, and usually containment or quarantine is sparingly used and applied to small geographic areas.
While its symptoms may be flu-like, COVID-19 (R0=2.5) is believed to be at least twice as infectious than the influenza virus (R0=1.5). This is in large part due to the novelty of the disease. Unlike the flu, there is neither a pre-existing exposure-derived immunity nor is there yet a vaccine to help shield the most vulnerable populations and front-line health care workers.
Given these factors, CNN’s Fareed Zakaria hosted the episode, “On GPS: How bad could Coronavirus get?” in which he interviewed former Centers for Disease Control and Prevention Director Dr. Tom Frieden. Zakaria explained the current exponential growth curve predictions that suggest infected individuals could reach as many as
3 million Americans in the first 33 days. Likewise, he cited national fatality predictions that range from 327 with just 1 percent of the U.S. population infected to more than 1.6 million with 50 percent infected.
There are ways to “flatten” this curve.
Modern medicine provides the tools that our ancestors lacked a century ago during the spread of the Spanish flu (1918-19) that can help slow the spread of viral infection. Ten days after its initial discovery, scientists sequenced the virus’s genome. A week after that, the first method to test for it was made available. With the test, people showing symptoms can know within 24-48 hours if they are infected.
However, as greater number of people become infected, testing contact circles of those testing positive will become a futile exercise, and so greater and greater numbers of individuals infected with COVID-19, who are carriers transmitting the disease silently to others, and are asymptomatic also will be invisible to the tallies. Others who exhibit only mild symptoms may choose not to be tested. Both groups will throw off the numbers more and more as time progresses. That is why social distancing and mandated closures are being implemented.
The time frame for the elimination of COVID-19 from activity around the U.S. will depend heavily upon people’s cooperation as a community over a sustained period.
DeWine tweeted on Sunday, “The choices you make will impact not just you, but your family, and those who you don’t even know. You have to make these individual decisions … The experts tell us that COVID19 may not peak until late April or May.”
But Ohioans and Americans alike are not sure exactly how long that cooperation might need to last and when the end might be in sight.
In England this weekend, Health Secretary Matt Hancock announced on BBC that in a few weeks the country will enact self-isolation for everyone over 70 years old for a period of four weeks.
Other British NHS estimates published Sunday in The Guardian are more dire, projecting active cases could continue for up to 12 months. Release of this government data suggests Americans should be prepared for the pandemic to continue for much longer than they might realize.
Still, even at a year, medical advances might mean this pandemic, with an estimated R0 of 2.5, could end at least entire year earlier than the Spanish flu pandemic 100 years ago, which had a smaller R0, just 2.0, as well as a significantly smaller global population size.